Your cart is currently empty!
Category: Physiotherapy
-
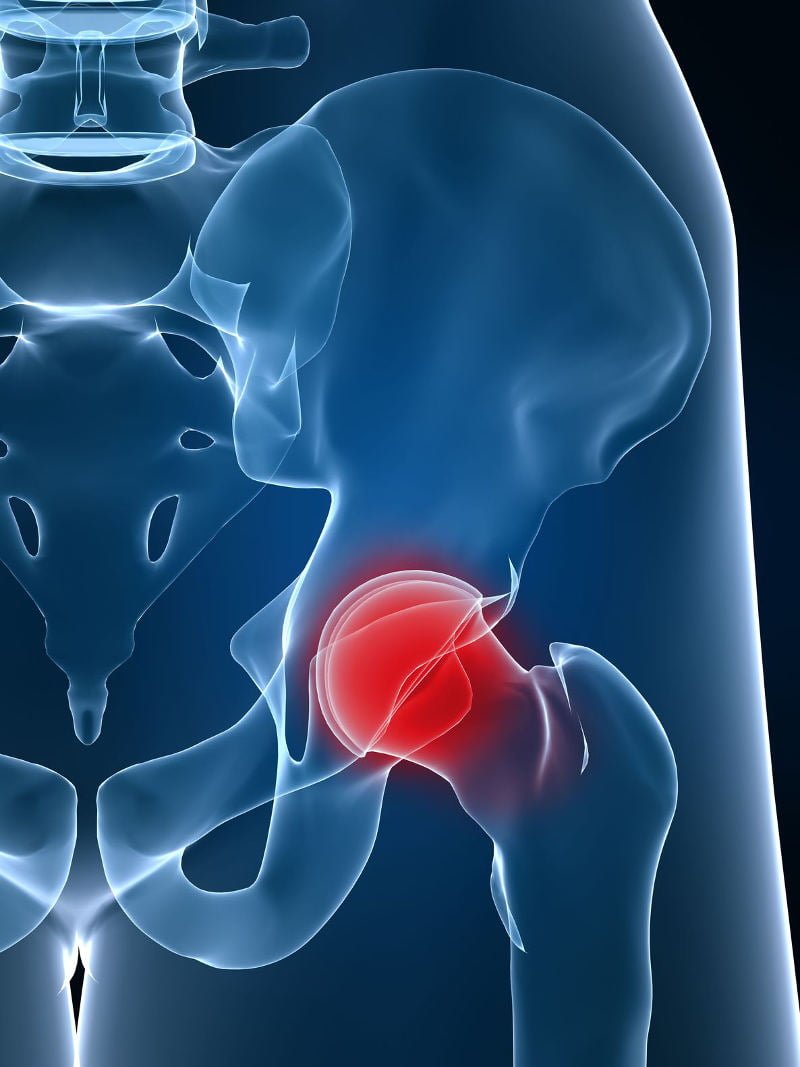
Fitness after Total Hip Replacement
Joint Replacement
- Surgical procedure for chronic severe joint pain
- Replacement with prosthetic
- Loss of muscle strength and mass has usually occurred
- Most frequent procedures are THR and TKR
Total Hip Replacement (THR)
- Frequent procedure in elderly population
- May be done for OA or RA or hip fracture
- Aim is to decrease pain and improve mobility and function
- Partial – (hemi-arthroplasty) or full
Management
Risk of dislocation for approx 3 to 6 months post-operatively
- Anterior approach – avoid extension and abduction and external rotation
- Posterior approach avoid flexion above 90 and adduction / internal rotation
Functional movements: what to avoid
- Sitting in a low chair (use wedge cushion)
- Lying on side – pillow between knees
- Avoid crossing legs over midline
Hip surgery recovery steps
- Carefully following the specific rehabilitation program provided your surgeon and his team
- Avoiding repetitive heavy lifting
- Avoiding excessive stair climbing
- Maintaining appropriate weight
- Staying healthy and active
- Avoiding impact-loading sports such as jogging, downhill skiing and high impact aerobics
- Consulting your surgeon before beginning any new sport or activity
- Thinking before you move
- Avoiding any physical activities involving quick stop-start motion, twisting or impact stresses
- Avoiding excessive bending when weight bearing, like climbing steep stairs
- Not lifting or pushing heavy objects
- Not kneeling
- Avoiding low seating surfaces and chairs
-

Carpal Tunnel Syndrome
Do you experience numbness of your thumb, index finger and part of your middle finger? Then you may have Carpal Tunnel Syndrome. Symptoms are often worse at night
The Carpal Tunnel is found on the palm side of the wrist. Several wrist tendons, blood vessels and the median nerve pass between the wrist bones and an overlying band of connective tissue through this area.
The causes of Carpal Tunnel Syndrome are still being researched and debated. The condition may be related to posture and biomechanics, for example sleeping with the wrists flexed and repetitive overuse activities have been cited as possible risk factors. Obesity, aging and genetics appear to be other possible factors in the development of this condition. It is more common in women, during pregnancy and in people with diabetes.
Like to know how you can help yourself heal? We can assist you with posture and ergonomic advice and gentle exercises and stretches. Some people will eventually require resting a splint, cortisone injections and / or surgery, because if left untreated permanent nerve damage and weakness of the hand may occur.
-

5 Ways to Counteract Sitting at Work

Five Ways to Counteract Sitting at Work
1. Micro-breaks
Eye breaks – every 20 minutes spend 20 seconds focusing your eyes on something 20 feet away from you (the 20 – 20 – 20 exercise). You should also blink the eyes a few times to lubricate them.
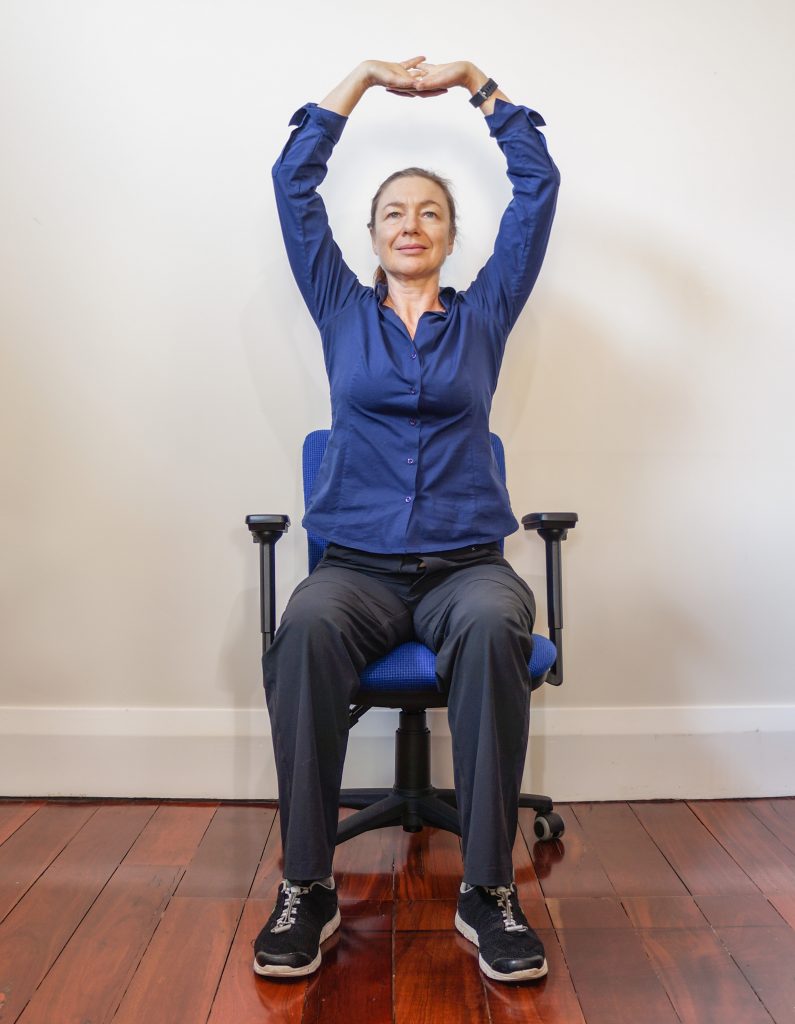
Deep breathing with an overhead stretch (sitting or standing). Interlace the fingers. Take a deep breath in as you raise your hands overhead and turn the palms towards the ceiling, looking upwards slightly. Repeat 3 times.
2. Walking breaks
Once every 30 to 60 minutes move away from your desk and walk briskly around the office. These short periods of activity that are simply part of your daily routine are known as ‘incidental exercise’. They are useful for preventing stagnation of the circulation. They help to raise your metabolic rate. There are many apps available to help remind you to get out of your chair.
You may simply get up, walk to another room and drink a glass of water or use the bathroom. It doesn’t necessarily mean that you stop working either. The break could be used, for example, to discuss something with a colleague or use the photocopier. Walking or jogging on the spot can provide an additional boost for your circulation. A short but brisk walk during the lunch break is another possibility.
3. Walking meetings and walking phone calls
Standing or walking during meetings helps increase activity level and lifts metabolic rate. If you use a mobile phone at work, make sure you have earphones with an inbuilt microphone. This way you can remain mobile while talking with colleagues or clients.
4. Walk to work
If you live too far from work to walk there, try parking your car further away and walking for the last 10 or 20 minutes. Taking public transport usually involves walking to and from the train or bus, which could be an improvement on taking your car. Research shows that we need an absolute minimum of 150 minutes a week of cardio-vascular exercise. This can be made up of any blocks of exercise that are at least 10 minutes long.
5. Active computer work stations and fit desks
Active work stations and fitdesks are a fantastic way to increase activity levels during the working day. Treadmill work stations allow you walk while you work. Cubii is an under desk elliptical that you can use while you work, without your knees hitting the desk. It has bluetooth connectivity so you can keep track of how far you have pedaled on your phone. Here is an interesting article that compares cycling desks with treadmill desks. The treadmill desks are more expensive but don’t interfere as much with productivity and the ability to work on a computer.
Stretches you can do at your desk
Stretches at work are helpful for reducing muscular tension and feelings of stiffness.
The following stretches can be done without leaving the vicinity of your desk. They target the most common places people feel tension after being at a computer.
READ OUR DISCLAIMER Please seek medical advice before commencing exercises, if you have a painful or medical condition.

Spine twist – Sitting in your chair, twist around to one side and look behind you, hold for a few seconds and repeat to the other side. This exercise helps stretch the shoulders, lengthen the back and fills the lungs with air, expanding the chest.

Forward bend – Sitting in your chair, slide your arms down your legs and let you head hang forwards, hold for 2 or 3 breaths in and out, then return to sitting. This gently stretches the lower back if it has been arching or compressed. It may help to help relieve lower back tension.

Pectoral stretch – Stand up, interlace the hands behind your back and raise the arms slightly towards the ceiling. The pectoral muscles at the front of the shoulders often become tight while using a keyboard. This exercise helps to lengthen them.

Back bend standing – Stand up, tighten the buttock muscles, use the hands to support the lower back and gently lean backwards, while looking upwards. Repeat several times without holding. This helps to counteracted a rounded lower back that can occur from slouching.

Stop sign stretch – Stretch one arm out in front of you with your elbow straight and your palm facing forwards, as in a policeman’s stop sign. Use the other hand to gently stretch the fingers back. Hold for a few seconds then repeat on the other side. This forearm stretch helps prevent Golfer’s Elbow (pain on the inside of the elbow).

Forearm stretch – Make a soft fist with one hand and extend it out in front of you, elbow straight. Turn the thumb side of the hand slightly towards the floor. Use the other hand to gently bend the wrist downwards. Do not do this stretch if you feel strain in the wrist. You may feel a stretch in the forearm if the extensor muscles which attach to the outside of the elbow are tight. Tight wrist extensors can lead to Tennis Elbow.
Also refer to our article “The Risks of Prolonged Sitting”
-

Physiotherapy for Tendinitis
Aims of Physiotherapy Treatment
In Tendinitis the aim is to reduce inflammation (for example using RICE) and you can expect to get better in approximately 6 weeks, although every case is different.
In Tendinosis it’s important to improve circulation and promote tissue healing. You should expect healing to take 3 to 6 months. Treatment may include cross friction massage, taping (for example with kinesio tape), trigger point acupressure or dry needle acupuncture, low level laser therapy and / or ultrasound.
Anti-inflammatory medications do not help tendinosis and cortisone injections may have an adverse effect, because they may actually inhibit collagen repair to the damaged tissues.
Enquire about our treatments for Tendinitis at Free2move.
-

Improving Posture

Improving Posture
Have you ever tried to improve your posture? How well did that work for you? If you are not satisfied with the results, consider attending Feldenkrais classes. The Feldenkrais Method can help you achieve comfortable and effortless posture through ingenious and mindful movement exercises.
The changes become integrated into your every-day life. Soon you will find yourself sitting, standing and moving in ways that you never imagined could be so easy or comfortable.
Body Scan Exercise in Sitting
Sit on a firm chair with your feet flat on the floor. Come forward in the chair a bit so you are not using the back rest. Sit normally and close your eyes for a few moments. Notice your posture. Stay there for a minute or two just observing yourself. Then open your eyes again.
When you observed your posture, what is the first thing that came into your awareness? What parts of the body did you sense? Perhaps you thought about whether you were sitting or standing up straight? You might have become aware or your head, neck and back. Perhaps you sensed your spine and checked its alignment. Maybe you tried to correct yourself. These are things many of us were taught to do growing up.
Consider that parts of your body that may not have been included in your awareness. Your hands and feet? Your chest and rib cage? Was your abdomen free to move with the breath? How long could you sustain this posture comfortably
3 minutes to Better Posture
Now try this short exercise with Ruthy Alon. Then go back to the sitting body scan above and feel the difference.
About Ruthy Alon
Ruthy is an international Feldenkrais trainer who studied and taught with Moshe Feldenkrais for over 20 years. It is hard to believe that in this video she is 85 years old. Ruthy is still teaching, a huge inspiration for those of us interested in healthy ageing.
4 Reasons why trying harder to sit or stand up straight doesn’t work
1. When we try to straighten the spine we often increase effort in the muscles of the back without releasing the flexor muscles in the front of the body. The result is one muscle group working against another. This causes spinal compression.
2. Some of us work so hard in our back muscles to maintain good posture that we end up bowed backwards, thinking that we are actually straight. This ‘military’ style of posture can lead us to be stiff and stuck in our movements. People who do this are usually unaware of it.
3. A common frustration in trying to improve posture is that the changes only work while you are consciously paying attention. As soon as you stop doing that, you slip back into old habits.
4. Yet another problem with this method is that the effort to straighten can result in restriction of the breathing.
4 Ways that Feldenkrais helps improve posture
1. Focusing on dynamic, not static posture
Moshe Feldenkrais described good posture as ‘the ability to move equally easily in all directions’. This is dynamic posture. By contrast, static posture may involve trying to hold yourself still when you are sitting or standing. This may cause breath holding. It’s also literally impossible be completely still. We actually maintain our balance in upright positions by using subtle swaying movements.
2. Reducing effort
As you learn where to let go of unnecessary effort, you will discover how to find more efficient support from your muscles and bones. Learning to move easily in and out of a particular position is just as important as maintaining good alignment.
3. Learning first while lying down
To learn a new way of supporting the body against gravity Moshe Feldenkrais first taught a variety of movement lessons lying down. The reason is that lying down makes it easier to reduce muscular effort. This helps you sense what you are doing more clearly so you can make small adjustments towards greater efficiency. It means you are less likely to fall into inefficient habitual patterns and postures.
4. Expanding the self-image
In the Feldenkrais Method you will learn to bring your attention to each part of the body that is involved in an action. You will learn how even seemingly unrelated parts of the body such as your hands, feet, eyes, ribs and hip joints can influence your posture. The more parts of your body that can be included in your self-image, the more clearly you will know what you are doing. In the words of Moshe Feldenkrais ‘When you know what you’re doing you can do what you want’.
“When you know what you’re doing you can do what you want” – Moshe Feldenkrais.
-

De Quervain’s Syndrome

De Quervain’s Syndrome
De Quervain’s syndrome refers to pain in two of the tendons which move the thumb – the abductor pollicis longus and the extensor pollicis brevis. Inflammation may occur where the tendons glide inside a fluid-filled ‘synovial’ sheath near the thumb-side of the wrist. Inflammation of this sheath is known as tenosynovitis.
Symptoms
Symptoms include pain on the thumb side of the wrist. Pain may extend up the forearm and a catching or snapping may be felt when moving the thumb. Sometimes there is localised redness and swelling. While often there is no definite cause, it is more common in new mothers (when it is aggravated by picking up their baby), middle-aged people, gamers, gardeners and in those with Rheumatoid Arthritis.
Treatment
Physiotherapy treatment may assist with relief of symptoms and addressing any known underlying causes. Interspersing rest and gentle exercises is usually required. Rest can be achieved by temporarily avoiding the aggravating movements and by using taping (strapping) or a splint.
At Free2Move we favour using stretchy ‘kinesio-tape’ such as Rocktape rather than using rigid strapping. Kinesio-tape does not restrict natural movement but improves sensory and movement awareness, while gently supporting the area.
Another treatment we often find effective at Free2Move is Low Level Laser Therapy (LLLT). Laser is thought to work by stimulating tissue healing while reducing pain and inflammation.
Preventing recurrence of the injury
Once pain has settled Feldenkrais or Pilates may be recommended to improve the way you move. In particular it is useful to look at the suspected aggravating movements. It’s helpful to find out how they can be performed with less effort, using the large muscles of the trunk to provide the power, with the small muscles of the hand being used to gently guide direction. This helps prevent the recurrence of the problem.
Severe cases
In cases where there is not an adequate treatment response, clients are referred back to their doctor, who may recommend a cortisone injection. In severe, unrelenting cases, surgery may be indicated.
-

Exercise, Imaging and Laser Therapy for Shoulder Pain

Exercise, Imaging and Laser Therapy for Shoulder Pain
A recent review of research on Low Level Laser Therapy (LLLT), also known as Cold Laser shows that it may be helpful in conjunction with exercise therapy for the treatment of shoulder pain. But should you see your doctor first? And do you need imaging, such as an Xray, Ultrasound or MRI? Read on to find out more.
Imaging and scans
Shoulder pain imaging can help determine whether you are likely to get quick results with Physiotherapy, or whether it would be better to seek an opinion from a specialist. Unfortunately, unnecessary referrals for these scans occur frequently and may not improve treatment outcomes. An experienced Physiotherapist will know when to refer you for a scan and when to persist with treatment.
Visiting your doctor
Should you decide to see your doctor first, do request a referral to see your Physiotherapist. Although a referral is not required in Australia, only 10 to 30% of patients who see their GP for shoulder pain are referred for Physiotherapy. This means you may need to be proactive and either ask for the referral or book a Physio appointment without a referral.
Specialist doctors may prescribe anti-inflammatory or analgesic medication, an injection or surgery. In most cases it’s better to try physiotherapy treatments such as exercise and Laser before seeing a specialist. However a good Physiotherapist quickly identifies clients who are not likely to make progress without medical procedures. Prompt onward referral in cases which are not responding saves you time and money and helps you get out of pain and return to normal functioning quickly.
Our Physiotherapists
At Free2Move our Physiotherapists use a variety of treatment techniques to promote quicker recovery from shoulder pain and dysfunction. These include taping or strapping, dry needle acupuncture, progressive range of movement and strengthening exercises and Low Level Laser treatment. Shoulder pain is a condition we treat every week in our clinic, so we are very confident that we can give you the best possible advice, minimising your recovery time. Because we consistently keep abreast of the latest scientific research , you can be sure that you will receive a high standard of treatment.
Research on Shoulder Pain and Laser Treatment
Conditions such as frozen shoulder (adhesive capsulitis), rotator cuff injuries (for example supraspinatus tendinitis) and sub-acromial bursitis respond may respond well to this combined approach.
Read More about research on shoulder pain and Low Level Laser Therapy.
-

Ergonomic Computer Work Stations

Ergonomic Computer Work Stations
Ergonomic computer work station set up is relatively simple. Doing things in the correct sequence is the key to getting it right. This helps minimise strain on your joints, muscles and soft tissues while working at your computer and reduces the risk of occupation overuse syndromes.
Adjust your chair first
- Adjust seat height
- Adjust the height of your back rest
- Adjust the back rest angle
- Adjust the seat slope
- Sit to the back of your chair
- Do you need a foot rest?
Adjust your monitor height next
- Adjust monitor height—eyes approximately 5cm below top of screen
- Do you need a monitor raiser?
- Position monitor arms length from your seated position
- If you have 2 monitors, position them to avoid twisting
Keyboard and Mouse
- Normal keyboard and mouse—suitable for most people
- Frequent use of numbers—numeric keypad
- Frequent use of mouse, but not numbers—mini keyboard
- An ergonomic mouse and or gel wrist / mouse support or a negative tilt keyboard may help some people
Laptops
- Avoid prolonged work (more than one hour)
- Use an external keyboard, laptop ramp, or plug your laptop into an external monitor
Other ergonomic considerations
- Your phone should be within close reach
- Wear a headset if you will be typing while on the phone.
- Use a document holder to reduce twisting of your neck.
- Excessive brightness, glare or inadequate light can strain your eyes
- Inadequate ventilation or being too cold or too hot at work can impair your performance.
Home visit and site visit services
Free2Move offer a home or site visit service to provide individual solutions to ergonomic computer work station issues
Please note: The above suggestions are a guide only. If you are experiencing pain or any other difficulties with your workstation, please seek the guidance of a health professional with an understanding of ergonomics.
-

Patellofemoral Pain

Patellofemoral Pain
By Alison McIntosh
Patellofemoral pain (and patellofemoral dysfunction) are a common causes of pain felt at the front of the knee. This pain originates from the joint between the patella (the kneecap) and the femur (thigh bone).
The patella usually glides/ tracks through the patella groove on the femur during flexion and extension of the knee. Compression is a natural component of this movement however an increase in the compressive force at this joint can result in patellofemoral pain. This can be caused by an alteration in the position of the patella (interfering with its smooth tracking during knee movements). An altered position of the patella is commonly a result of quadriceps (front thigh muscle) imbalance.
The most common imbalance occurs when the pull of the outer quadriceps muscle (Vastus Lateralis) is too strong compared with the pull of the the inner quadriceps VMO (Vastus Medialis Obliquus) which is often too weak. If the lateral structures of the knee (Iliotibial band and Retinaculum) are very tight this adds to the problem, which is known as ‘patella maltracking’.
Common signs and symptoms of patellofemoral pain:
- Pain underneath the kneecap
- Knee pain with rising to standing from a seated position
- Knee pain associated with prolonged knee flexion (eg sitting in the movies/ on an plane)
- Knee pain with climbing and particularly descending stairs
- Knee pain with running , hopping, squats, lunges
Common causes of patellofemoral pain:
- Over pronation of the feet ‘dropped arches’ as a result of
- poor foot wear (inappropriate arch support)
- a genetic pre-disposition (possibly a family history of hypermobility ) or
- as a result of poor gluteal strength (important in maintaining a neutral lower limb alignment)
- Over loading of the joint as a result of
- biomechanics (one stronger more dominant limb)
- occupational causes
- sporting limb dominance
- Recent changes to an exercise regime i.e.
- recent commencement of running
- alteration of fitness regime to include squats, lunges, hill or stair training
- recent increase in intensity of a training program
Diagnosis:
A diagnosis of patellofemoral pain or patellofemoral dysfunction is usually made without the need for medical imaging. A physiotherapy assessment will frequently involve:
- Specific orthopaedic testing of the patello femoral joint
- Biomechanical analysis
- Gait analysis
- Functional testing of the knee, ankle hip and pelvis
- Knee ligament testing to aid in identifying any additional knee ligament or cartilage involvement
- Hip and lumbar spine testing to aid in identifying any referred pain
- Functional assessment to determine strength/balance/alignment
Treatment:
The first aim of treatment is usually to reduce pain in the short term. At Free2Move we frequently use a patient specific combination of the following modalities
- Acupuncture
- Soft tissue massage
- Joint mobilisations
- Taping
- Neuro muscular re-education through the Feldenkrais Method
- Foot wear advice and arch support taping
- Exercise/training modification
Secondly, treatment of patellofemoral pain would aim to restore efficient bio-mechanics, improve function and if required focus on sport specific rehabilitation. This may be achieved using:
- Feldenkrais Method
- Clinical Pilates
- Patient specific home exercise program ultimately aiming to reduce the likelihood of any re-occurrence of the problem

